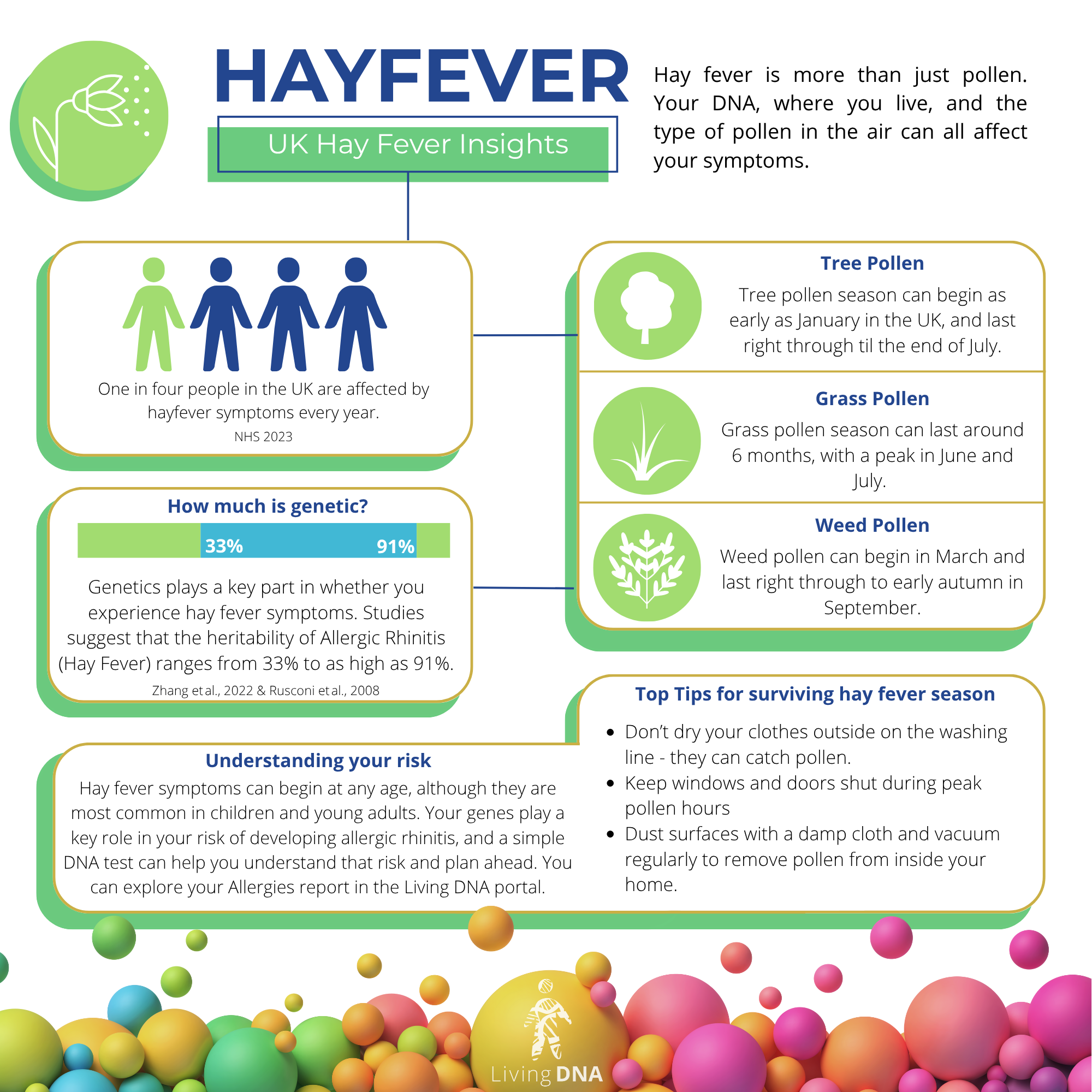
It’s that time of year again. The sun is shining, flowers are blooming, and for millions of people across the world, the sneezing, itching, and sniffling has begun, or even intensified. Peak hayfever season lasts from March until September in the UK, but seasonal allergies can start as early as January.
While some breeze through spring and summer unbothered by pollen, others are left battling with a constant runny nose and sore eyes. Why do some people suffer so much more than others? Is it just down to luck?
In a world where climate change is extending and intensifying pollen seasons, understanding your personal allergy risk is more important than ever. And one of the key factors in that risk is your genes.
So What Is Hayfever?

Also known as allergic rhinitis, hay fever is an allergic reaction to airborne particles, most often pollen from trees, grasses, and weeds. Other triggers can include dust mites, pet dander, and mould spores.
When someone with hay fever encounters one of these allergens, their immune system mistakenly sees it as a threat. This sets of a defensive reaction that leads to all-too-familiar symptoms that include:
Sneezing
Runny or blocked nose
Itchy eyes, ears, or throat
Headaches and fatigue
Although the symptoms can feel like a cold, hay fever is not caused by a virus. It’s your immune system overreacting to something harmless in your environment.
According to the NHS, around one in four people in the UK experience hay fever symptoms each year. That’s a lot of us reaching for tissues and antihistamines as soon as that pollen count starts to rise!
The Genetics of Allergies: What We Know

Allergies often run in families, and hay fever is no exception. If one or both of your parents suffer from allergic conditions, your own risk increases significantly, but it’s not as simple as inheriting a single “hay fever gene.”
Allergic rhinitis is polygenic, which means that multiple genes contribute to your likelihood of developing symptoms. These genes influence how your immune system recognises and responds to potential allergens.
A key player is the HLA (Human Leucocyte Antigen) gene group. These genes help your immune system to distinguish between what is harmful and what isn’t. In some people, specific HLA variants are linked to an increased sensitivity to allergens, including a well documented association with olive pollen allergy, common in Mediterranean climates.
This exaggerated immune response is your body’s way of being a little bit over cautious, but it often causes more harm than good.
Environment + Genetics = Your Personal Risk

While your genes provide the blueprint, your environment also helps to shape your response to allergens.
Air pollution, early childhood exposure to allergens, seasonal changes, and even your gut health can influence whether your genetic predisposition will turn into actual hayfever symptoms. In fact, it’s possible to develop hay fever even if you don’t carry those high-risk genetic markers, especially if your immune system has been primed to overreact by repeated exposure to allergens in your environment.
In other words, your hay fever risk is a delicate balance between nature and nurture. Understanding both can give you a more complete picture of why your symptoms occur, and how best to manage them.
Genetic Testing and Understanding Your Risk

Living DNA offers an allergies test, under the Health menu in your portal. It looks at genetic markers involved in hayfever as well as other common allergies. While it isn’t a medical diagnosis, it can be a powerful tool to increase your self-awareness; helping you to recognise patterns, ask informed questions, and take proactive steps in managing your own health.
Once you’ve taken a Living DNA test or uploaded your raw data, visit the store in your portal to learn more.
What Can You Do?
Knowing that you could be more sensitive to allergens can give you a head start on managing your symptoms. There are ways you can minimise your discomfort during hayfever season:
Monitor the pollen forecast and limit time outdoors when counts are high, if you can.
Use HEPA air filters at home to reduce pollen exposure inside your house.
Dry clothes indoors to avoid bringing pollen in from outside.
Rinse your hair and face after time outdoors, to reduce trapped pollen.
Use over the counter treatments like antihistamines or nasal sprays, especially if recommended by a healthcare professional. *
Most importantly, you can advocate for yourself. If your symptoms are affecting your quality of life, speak with a GP about allergy testing or treatment options. Armed with your genetic insights, you’ll be better prepared to discuss potential causes and solutions.
Explore Your Allergy Report with Living DNA
Our genetic health tests cover more than just allergic rhinitis. They explore a range of traits related to your nutrition, fitness, sleep, and personality. If you’ve taken a Living DNA test, your allergies report is available through the store in your portal.
* Always follow the instructions provided with any treatment, and consult your doctor or pharmacist before starting any new medication.